© 2017 Roy Benaroch, MD
Linus Pauling was a brilliant scientist. He won the Nobel Prize in Chemistry in 1954 (and, later, a Nobel Peace Prize for his work towards nuclear disarmament.) In the later part of his career, he became convinced that megadoses of vitamins, especially vitamin C, could ward off upper respiratory infections and other ills. Studies have never supported those claims. But maybe he was only off by one letter of the alphabet.
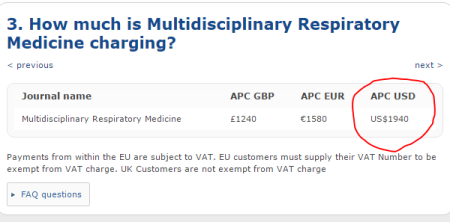
A recent, large study from the BMJ provides solid support for the use of vitamin D – not C, but D – supplementation to prevent ordinary colds and other respiratory infections.
There’s been some inkling that this might be the case. We know that vitamin D, separate from its role in calcium metabolism, has an important part to play in our immune response to infections. It supports the production of built-in antiviral and antibacterial peptides, and helps immune cells make germ-destroying oxygen and nitrogen compounds. Population studies that have shown an increased susceptibility to colds among people who are immune deficient.
What we haven’t had, until now, is a convincing study from an experimental perspective. If we give vitamin D, does that really prevent colds?
What these authors did was impressive. They collected the raw, patient-by-patient data from 25 previous clinical trials of vitamin D, and combined all of that into one mega-study with about 11,000 participants. All of the patients had to have been randomized to either vitamin D or placebo, and rates of respiratory infections tracked going forward. Most of them had blood tests to assess their levels of vitamin D before the trials began.
The bottom line: vitamin D supplementation decreased the risk of a cold by about 12%. That doesn’t sound very high, but on a population level, we’re talking about a lot of infections. And: among those that had low vitamin D levels, the effect size was much larger, about 40%. Vitamin D supplementation was more effective in preventing colds with a daily dose rather than just bolus dosing once in a while.
Who’s low in vitamin D? Based on my experience looking and blood tests from children and teenagers, all of our children are low. Seriously. The only time I see blood tests reflecting a normal or high vitamin D level, it’s in someone already taking a supplement. Our children (us, too) aren’t spending enough time outside to make the vitamin D we need.
The study also found no downsides to ordinary supplements. There were no significant side effects or problems. We’re talking, here, about ordinary doses of probably 400-2,000 IU each day. There’s really no reason to take any more than that, unless there’s a problem with vitamin absorption or some other unique medical issue.
Vitamin C, Airborne, zinc, echinacea – none of these have held up to scrutiny. None of those help prevent people from getting respiratory infections. If you want you and your children to get fewer colds, there are only a few strategies that genuinely work. Stay away from sick people, keep infants out of group care, wash hands frequently, and immunize against influenza and other respiratory pathogens. And, maybe, enjoy a little more time in the sun, or take a vitamin D supplement every day.




 No. They can’t, and they don’t. They can sometimes cause a little fever or achiness, but that is not the flu—and anyone who’s actually had the flu will tell you that these mild symptoms after a flu vaccine are pretty much nothing. Sometimes, right after a flu vaccine, someone does get the flu—that’s because we’re giving flu vaccines during flu season, and if you don’t get it in advance it can’t protect you. The vaccines take about 3 weeks to work. If you catch influenza right after getting the flu vaccine that’s called “bad luck” or “bad planning”, not “bad vaccine.”
No. They can’t, and they don’t. They can sometimes cause a little fever or achiness, but that is not the flu—and anyone who’s actually had the flu will tell you that these mild symptoms after a flu vaccine are pretty much nothing. Sometimes, right after a flu vaccine, someone does get the flu—that’s because we’re giving flu vaccines during flu season, and if you don’t get it in advance it can’t protect you. The vaccines take about 3 weeks to work. If you catch influenza right after getting the flu vaccine that’s called “bad luck” or “bad planning”, not “bad vaccine.”













Recent Comments